in
HEART
The Google Maps for
Cardiac Ablation
By Gergana Koleva
inHEART is on a mission to show that innovation in cardiovascular medtech comes not only from bringing cutting-edge technology, but also from marrying specialty domains rarely seen together: medical imaging and cardiac electrophysiology. The offspring of this unexpected union, orchestrated by the Bordeaux-based startup, is a lifelike 3D digital model of the heart that will enable cardiologists to do away with invasive diagnostic catheters and plan a detailed ablation strategy before the procedure.
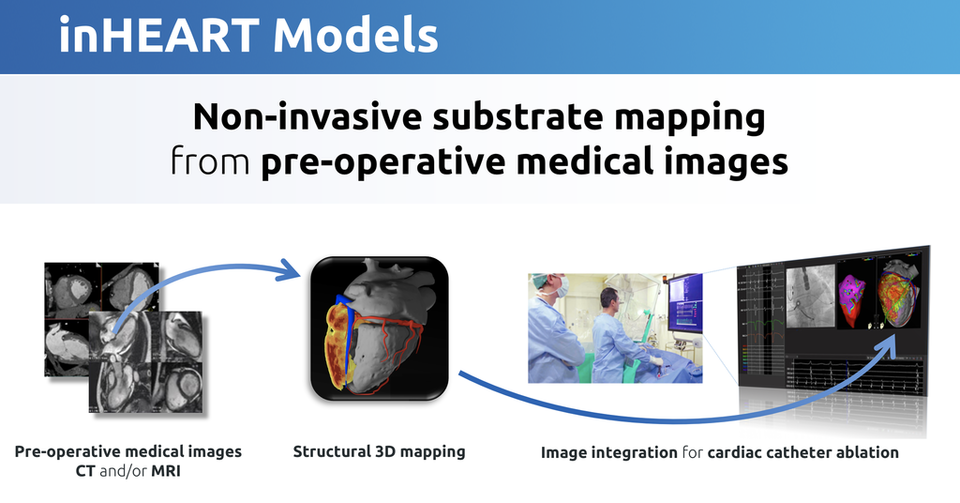
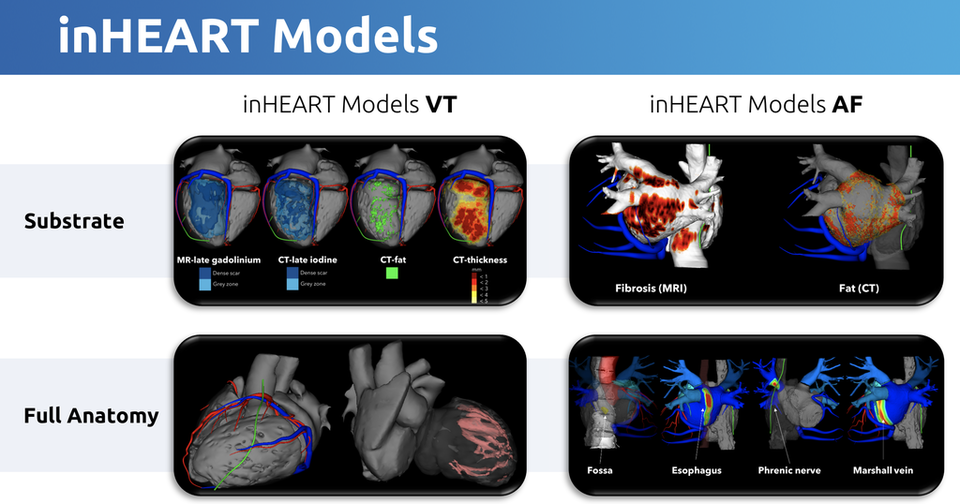
inHEART, a spin-off from the prestigious French research institutes IHU Liryc and Inria, is reinventing the relationship between cardiac electrophysiology and medical image analysis. Its cloud-based SaaS solution transforms pre-operative scans (CT and MRI) into 3D digital twins of patients´ hearts and infers the origin of abnormal electrical activity from the underlying data. This level of detail is made possible by the company’s proprietary AI algorithm, trained on more than 2000 cases to detect connections between cardiac imagery and corresponding pathologies, which permits operators to virtually map out interventions down to the most minuscule detail before they have even met their patients.
The concept of using medical imaging scans as a foundation for 3D heart models that depict electrical abnormalities stems from the view that invasive procedures such as cardiac catheter ablations are due for an upgrade. An upgrade that aspires to higher precision and that is based on making interventional workflows faster, safer, and more efficient while bringing upstream the process of their planification. Traditionally, decisions such as how much scar tissue to ablate have been left to cardiac electrophysiologists to make intra-operatively, once they have begun an intervention and observed in real time the heart region they are repairing. But as inHEART´s technology renders a literal digital reconstruction of the heart with the precise visualization of structural substrate for both atria and ventricles, the company hopes to bring this planning stage upstream.
“Currently, most of the procedure time is used for electrical diagnosis and identification of ablation targets, and only a small part of the time is for the ablation therapy itself. By doing the diagnosis before the intervention based on pre-operative imaging, we envision being able to get rid of complex and lengthy intra-operative diagnoses,” says inHEART CEO Jean-Marc Peyrat. Emphasizing this point, he notes that it could reduce the average time it takes to perform an ablation, which lasts between four and six hours, down to two hours.
“It is the Google Maps of cardiac catheter ablation. Catheters have been enhanced with 3D localisation systems, a bit like the GPS in a smartphone, but imagine yourself using Google Maps without a map and just your GPS coordinates. You would need to reconstruct the map of the city you are visiting while walking around and discovering it, without knowing where the best touristic sites, restaurants and shops are. inHEART provides this missing map to the cardiologist,” he says.
The big idea
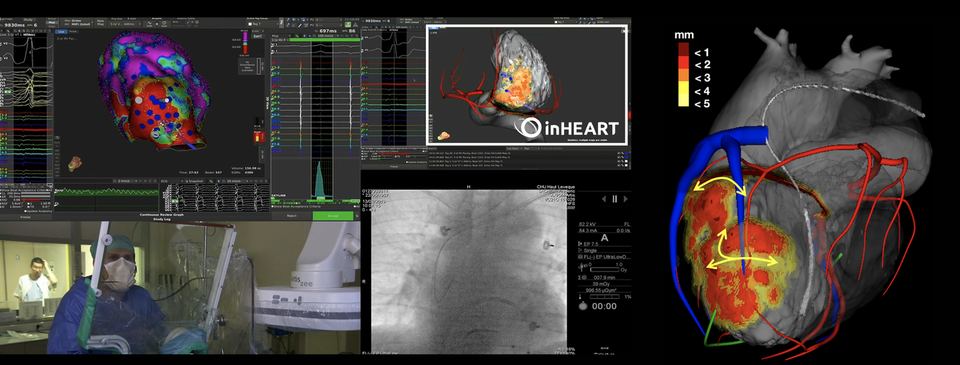
Using inHEART´s solution requires a clinician to load deidentified DICOM images to a secured company server. Once the data are uploaded, trained case analysts process the images into digital recreations of anatomically identical 3D models. The models can be annotated and exported from the cloud back into the local enterprise system from which their data originated so that they can be joined with the patients´ personal details, which never leave the hospital to begin with. When completed, the process enables interventional cardiologists to navigate their instruments in real-time following the heart´s geography as intricately mapped by the models, rather than depending on in situ discoveries and subjective judgment.
The inspiration for this technology came from a collaboration between IHU Liryc and Inria dating back to 2010. Since then, a multidisciplinary team of radiologists, cardiologists, and computer scientists had worked to develop medical image processing tools to better diagnose, predict and treat cardiac electrical disturbances that are at the root of arrythmias leading to sudden cardiac deaths, strokes, and heart failures. inHEART was born out of that team´s efforts to create a tangible solution that vividly communicates the relationship between structural abnormalities observable with imaging and electrical abnormalities observable with invasive mapping (intracardiac catheters).
“The opportunity to analyse imaging and electrophysiological data in the same environment enabled the team to solve the scientific challenge to link many imaging features to abnormal electrical activity,” says Peyrat.
How it works
In practice, the crowning achievement of this partnership – embodied in inHEART´s pre-procedural imaging and 3D modelling solution – translates into making unnecessary operator- and equipment-dependent intra-procedural electrical measurements, as well as the induction of arrhythmia in order to map the structural information of the heart. By integrating medical images during the procedure, inHEART´s cloud-based service has shown in pilot studies to reduce from 40% to 20% the risk of unsuccessful procedures that require a secondary intervention, which in turn leads to lower costs for payers and patients. In addition to also halving the procedure time from four or more hours, the company´s innovation has the potential to make redundant the use of costly diagnostic catheters, which results in further savings of at least $2,000 per typical ablation procedure, according to Peyrat´s estimates.
inHEART technology developed for cardiac ablation could also be used to which patients actually need to undergo the implantation of a defibrillator and which are not candidates for it.
“The risk stratification process to decide whether or not to implant a defibrillator is still based on very global information that is the left ventricular ejection fraction – and it has poor results. Patients are implanted both too much (only one third really need it) and not enough (nine-tenths of those who need it are implanted). We strongly believe that this risk stratification could be improved with more refined analysis of cardiac imaging such as the one we developed to characterise the myocardial tissue,” says Peyrat.
Savings and efficiencies
Looking to the future, inHEART anticipates that the arrival of non-invasive ablation will make even more obvious the choice of non-invasive diagnosis. Peyrat also predicts that major players today may see their fortunes shift if they don´t keep up.
“Our technology will be a cornerstone of non-invasive ablation with radiotherapy. If you can ablate non-invasively, you need to be able to define the ablation target non-invasively as well, which is what we can provide. Non-invasive ablation has been of growing interest for the research community. There is a long way before we radiotherapy ablation in the clinical routine, but when it will come, it could be disruptive for Abbott, Boston Scientific or Biosense Webster, whose equipment would not be necessary anymore,” he says, referring to three of the market leaders in the cardiac electrical measurement space. And he justifies it simply: “inHEART brings a new way of looking at cardiac electrophysiology: before having an electrical disorder, there is often structural disorder, so in the future, we envision that cardiac catheter ablation will be guided purely based on pre-operative imaging without the need of a diagnostic catheter.”
The road ahead


It is the Google Maps for cardiac catheter ablation. Catheters have been enhanced with 3D localisation systems, a bit like the GPS in a smartphone, but imagine yourself using Google Maps without a map and just your GPS coordinates. You would need to reconstruct the map of the city you are visiting while walking around and discovering it, without knowing where the best touristic sites, restaurants and shops are. inHEART provides this missing map to the cardiologist.
Jean-Marc Peyrat, CEO, inHEART
By eliminating highly invasive intermediate steps, inHEART´s cloud-based service reduces from 40% to 20% the risk of unsuccessful procedures that require a secondary intervention, which in turn leads to lower costs for payers and patients. In addition, it halves procedure time from four or more hours and makes redundant the use of costly diagnostic catheters, which results in further savings of at least $2,000 per typical ablation.