Marrek
Improving AF
Ablation Success
Marrek’s ability to identify fibrosis and quantify the extent of cardiac tissue damage promises to help cardiologists achieve better outcomes for their atrial fibrillation patients.
By Stephanie Kreml

Nassir F. Marrouche,
Marrek founding member
Fibrosis in the myocardium is emerging as an important factor for how effectively electrophysiologists can treat cardiac arrhythmias. Marrek, an innovative company providing the Merisight service, offers an analysis of cardiac fibrosis to help electrophysiologists identify the location of pre-existing tissue damage.
“Fibrosis is associated with many heart diseases, including congestive heart failure, cardiomyopathies, and arrhythmias,” says Dr. Nassir F. Marrouche, one of the founding members of Marrek and current Cardiac EP Director at Tulane University School of Medicine. “Therefore, the quantitative measurement of fibrosis is important in patient diagnosis and treatment planning.”
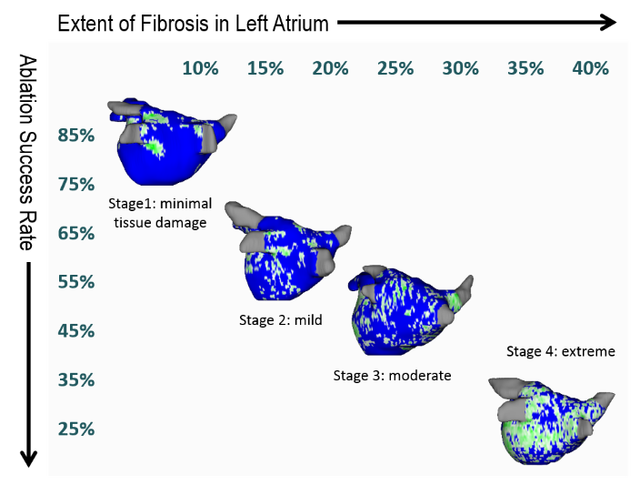
The overarching concept is that doctors simply need more and better information about the extent and localization of tissue damage in their patients’ hearts before treatment. This contributes to the poor outcomes seen after ablation procedures for atrial fibrillation (AF). Currently, doctors on average only have ~50% chance of success in treating AF in their patients using a variety of current ablation techniques.
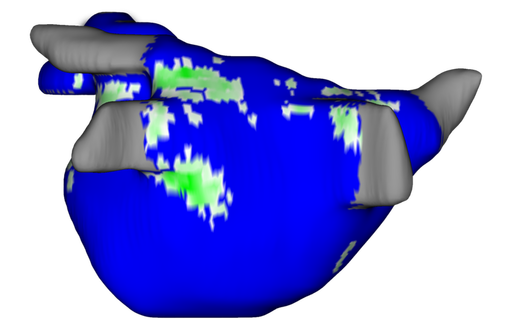
Marrek was founded to make an impact in these statistics. Utilizing non-invasive MRI, Marrek’s proprietary technology service (Merisight™) tells doctors where their patients’ tissue damage is located in the heart as well as the extent of damage.
Marrek’s analysis of delayed-enhancement cardiac MRIs can assist electrophysiologists in planning their catheter ablation procedures. “The application of Marrek’s technology for patients with cardiac arrhythmias has been clinically studied and published in prominent peer-reviewed journals,” says Nathan S. Burgon, VP Services & Innovation and Managing Director. “Of significance were the results from a multi-center study (known as DECAAF) reported in the Journal of the American Medical Association. The results demonstrated that ‘fibrosis, estimated by delayed-enhancement MRI, was independently associated with the likelihood of recurrent atrial fibrillation arrhythmia’ and that patients with less fibrosis, ascertained by Marrek, had better ablation success.”
In fact, the DECAAF (Delayed-Enhancement MRI Determinant of Successful Radiofrequency Catheter Ablation of Atrial Fibrillation) study also showed that “one of the most important predictors of ablation outcome was the extent of ablation of the fibrotic tissue,” Burgon explains. “That is, the more fibrotic tissue that was ablated, the better the outcome.”
To use the service, Marrek provides optimized sequences and protocol training to ensure the highest quality delayed-enhancement cardiac MRI images. Delaying imaging after administration of contrast allows the contrast to accumulate in the fibrotic tissues for identification and quantification. “MR images can be directly pushed to our web portal from the MRI scanner and be sent to Merisight processing,” says Burgon.
He continues, “Once the MRI is submitted on the secure web-based platform, our technicians use FDA-approved software to process the images and create visualizations of left atrial enhancement.” Merisight then reports these models and relevant data back to the patient’s cardiology team. The reports are usually available by the next day, but Marrek can support same-day turnaround requests.
“[There is] a new methodology to personalize AF treatment,” Marrouche states. “This offers additional insight into treatment and outcomes that in the past have relied principally on clinical classification. This new information and quantification of fibrosis better accounts for the progression and myopathy of each AF patient.”
The Merisight service has the potential to decrease ablation procedure times by making intra-procedure catheter-based mapping more efficient. “The models we create are compatible with and can be seamlessly integrated with electro-anatomical mapping systems to create a combined, single image, used in catheter ablation,” says Burgon. The integrated model equips the ablationist with tissue information, for first-time and re-do ablations, intra-procedurally to simplify and increase the overall efficacy of the procedure.
While there are other companies using various approaches to improve cardiac imaging, Burgon is optimistic about this growing field. “Our strictest competition is the current diagnostic and treatment standards including CT scans, standard MRI, or no screening or treatment at all,” he says. “The development of direct competition in the market leaves [us with] the burden of proof, validation of service, and education. Creating awareness and influencing treatment is an opportunity to drive interest and continue to establish Marrek’s edge of being first to market with an FDA-cleared solution.”
Using Marrek’s technology, the DECAAF study showed patients with less heart tissue damage have better ablation success. But for those patients with more fibrosis and tissue damage, Marrouche intends to improve their outcomes as well by building on the findings of the original study as the principal investigator of DECAAF II. “These data have the potential to expand the ablation treatment market for AF patients while also improving patient outcomes,” he explains.
The DECAAF II study is currently underway and can demonstrate Marrek’s effectiveness in identifying fibrosis for ablation targets. This prospective, randomized clinical trial will compare conventional pulmonary vein isolation (PVI) ablation alone to PVI plus fibrosis-guided ablation using the Merisight platform. The study aims at modifying and improving persistent AF management guidelines by evaluating targeting DE-MRI detected atrial fibrosis during AF ablation and its related effect on procedural outcome.
“We believed that many treatment decisions were being made with little understanding of the tissue structure of a patient’s heart,” says Marrouche. “Now, MRI tissue data can be directly used in guided ablation treatment resulting in improved patient outcomes and an overall lower total care cost.”
Predicting Ablation Success
Personalizing AF Treatment
Predictive to Prescriptive

The models we create are compatible with and can be seamlessly integrated with electro-anatomical mapping systems to create a combined, single image, used in catheter ablation.
Nathan S. Burgon, VP Services & Innovation and Managing Director.
Doctors simply do not have enough information about the extent and localization of tissue damage in their patients’ hearts before treatment.
